We might well be moving towards the end game for the coronavirus and it’s associated disease COVID-19.
What is becoming pretty clear is that for a full economic recovery people need to be in close proximity to each other without fear of contracting Covi-19.
Any current discussions about a vaccine for coronavirus are always guarded ones nowadays and include the phrase “we might never have a vaccine”.
Whist this is perfectly true the one thing that this global viral pandemic has given us is an opportunity to completely revise how vaccines are developed worldwide simply as a result of funding.
The sticking point for developing vaccines has changed dramatically over the last six months following the emergence of the virus in Asia . One thing that can’t be changed is the time taken to do the three stage mandatory trials and tests to ensure that the vaccine both works and is safe. Having said that both China and Russia have approved vaccines for their countries seemingly without full safety protocols in place.
The beginning of last year saw new methods of developing vaccines being investigated, the concept existed before that however, the big stumbling block was getting companies to invest money into new methods of development.
All that changed when the coronavirus pandemic started sweeping the globe, with governments all over the world happy to throw millions of pounds in the direction of the pharmaceutical companies if they cold find something to eradicate the virus.
That is the problem with vaccines their viability of embarking on development was always questioned because delivery was in a timeframe that was often outside the length of the outbreak.

One technique that fits perfectly into this category was mRNA vaccine technology and its development was years away from perfection until recently. The standard method of dealing with a viral pandemic would be some version of lockdown and it’s associated social distancing in order to “flatten the curve” this was the approach as developed in the mid 2000’s. This method can only restrict an outbreak down to levels that are manageable. The only way to eradicate the disease is to develop a vaccine.
At that time mRNA viruses (messenger RNA) were rare and only a very few had ever entered into clinical trials. These mRNA vaccines stem from the late 1980’s when research was looking at developing a method of cheaply synthesising both DNA and RNA strands.
Messenger RNA carries messages around to parts of our body but it only last hours or days then wears off.
It carries a specific meesage for DNA to do things, but the problem had always been that synthetic RNA when injected into a living being would simply kill the specimen. All this changed in 2004 when by tinkering with the RNA in such a way so that it doesn’t trigger human immune systems to self destruct.
Prior to investigating an mRNA coronavirus vaccine mRNA was being studied as a way of combating cancer. It is however extremely versatile.
The big advantage of mRNA vaccines is that once a new viral gene was identified it can be targeted using the mRNA to produce a vaccine very quickly. You simply need to identify the gene.
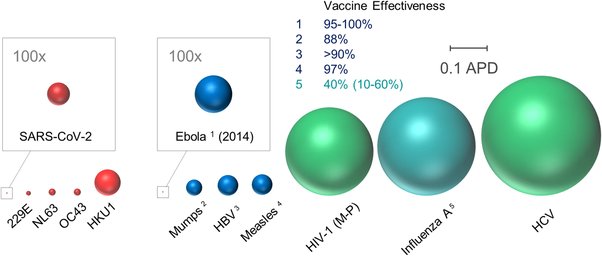
Once this was done you could target a whole range of viruses including rabies, Ebola and HIV and of course coronavirus. The brilliant thing about mRNA vaccines is that once you have developed a vaccine for say Ebola all you need to do is swap Ebola for coronavirus as the target gene and and then just run the trials for safety and efficacy.
Since China had already sequenced the coronavirus genome it was very easy to swap targets. It was also cheap as each genetic letter letter cost just 0.07p to purchase.
The second big advantage with mRNA vaccines and probably the one that make it so attractive is ease of manufacture. Currently even if an approved vaccine were in existence the world’s manufacturing capacity is only half of what would be required produce enough vaccine to immunise the worlds population and so eliminate the virus worldwide.
 Traditional vaccine manufacturing is more of an industrial process than one that occurs in a lab. It involves multiple stages, the flu vaccine for example involves cultivation in eggs followed by harvesting the vaccine from those eggs and is both a costly and time-consuming process. These mRNA vaccines mean that you can reproduce millions of doses from a standard laboratory research facility.
Traditional vaccine manufacturing is more of an industrial process than one that occurs in a lab. It involves multiple stages, the flu vaccine for example involves cultivation in eggs followed by harvesting the vaccine from those eggs and is both a costly and time-consuming process. These mRNA vaccines mean that you can reproduce millions of doses from a standard laboratory research facility.
expanding manufacture on a large scale is straightforward it’s only really complicated by the final purification step. We must of course remember that manufacturing the vaccine is only part of the story and any one link in the chain that fails can halt production. For example earlier in the year the concern was that there was any issue with the sourcing of the specialist glass needed to make vials for injectable doses. The vaccine would have been in abundance but there was nothing to put it in!
Currently the big players in the mRNA vaccine stakes are Moderna in the US, Imperial College in the UK and BioNTech in Germany.
Despite there being a number of potential hold-ups in the production it does seem that mRNA vaccines are a straightforward cheap and fast way of producing a vaccine for a newly discovered virus. If we can get one of the current mRNA vaccines tested and into production it does seem that these vaccines are the best way to counteract potential viral epidemics and pandemics worldwide.