Since the widespread use of mRNA vaccines, vaccine breakthrough and new variants have been bombarding the media all the time. The emergence of new variants quickly exhausted the Greek alphabet and some variants like omicron are even proven to be capable of dodging the immunity against the original version. While these news are undeniably true, they are a bit misleading as one can easily make a conclusion that the primary reason for the failure of herd immunity is due to the rapid mutations of the virus, as exemplified by influenza.
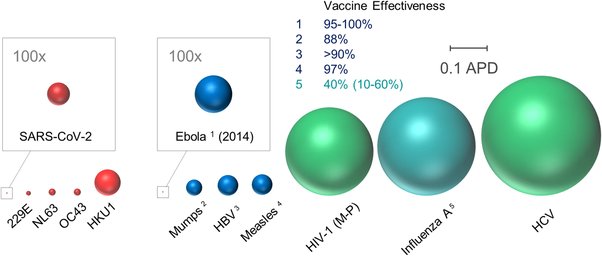
While influenza is an archetypical virus which mutates rapidly to dodge our antibodies and infects us over and over again, influenza virus is not an outlier among respiratory viruses. Many respiratory viruses like rhinovirus, coronavirus, parainfluenza virus and RSV are capable of causing repeated infections. It would be extremely unlikely that the respiratory tract enriched the most mutative viruses in the world. Indeed, many respiratory viruses including the 4 endemic coronaviruses don’t exhibit a high antigen variability. Moreover, researchers found that people infected with coronavirus previously can be reinfected when challenged with the original strain a year later (because endemic coronaviruses only cause minor colds, human challenge studies are acceptable), which indicates a short duration of immune memory. On the other hand, some respiratory viruses like measles and smallpox do confer long-lasting sterilizing immunity either naturally or by vaccination, which enables us to cut off their transmissions and even eradicate them by massive vaccinations. So besides antigenic variability, there may be other reasons for the different outcomes.
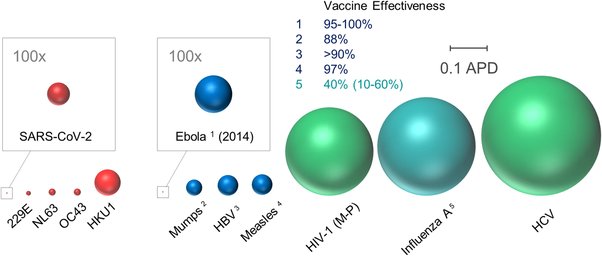
One key difference between influenza-like and measle-like viruses is their replication strategies. Influenza virus has a very simple replication cycle. Once inhaled, influenza virus infects the respiratory epithelium via the airway. The infected cells in turn shed new viruses back to the airway. Measles OTOH is much more complex. When measles virus enters the lungs, it does not infect the epithelial cells directly because these cells lack the receptor at the apical side (the side facing the airway). Instead, the virus is picked up by lung macrophages and carried to lymph nodes. Measles virus is capable of infecting a broad spectrum of white blood cells, so it quickly multiplies to huge number inside the lymph nodes and disseminate throughout the body via the blood circulation. Once in the blood, measles virus can infect the respiratory epithelium via the basolateral side (the side facing the bloodstream) and exit via the apical side. Compared with atypical respiratory viruses like measles, smallpox and Nipah, influenza-like viruses are more restricted to the respiratory tract and rarely invade other parts of our body. They also cause milder diseases (unless the virus has a strong tendency to invade the lower respiratory tract as is the case of H5N1, H1N1(1918) and SARS-CoV-1) and spread faster (viruses like influenza and SARS-CoV-2 can be infectious within 2 days even before the symptoms emerge).
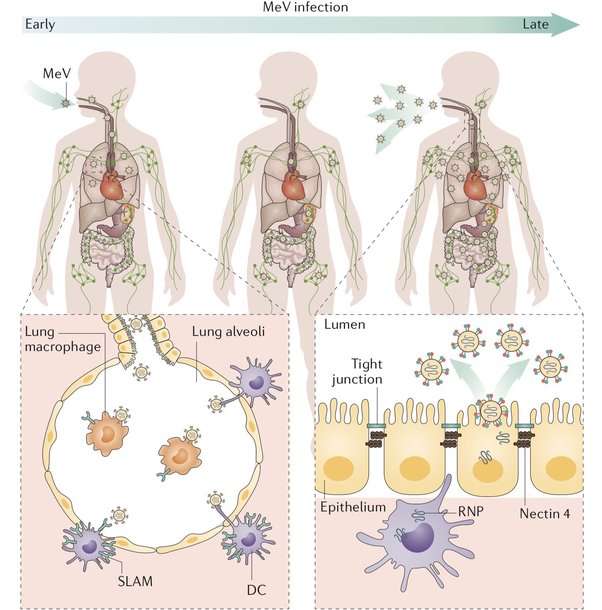
The difference between their replication strategies may play a bigger role in breakthrough infections. Because measles must multiply in the lymphatic system for a few days before infecting the respiratory tract and the lymphatic system has abundant memory T cells and B cells, there is a wide time window for them to activate and eliminate the infection before it can spread. Influenza and SARS-CoV-2 are infectious within two days, which means by the time the immune system is awakened, the viral transmission may have been done. The respiratory tract is also a bit immunosuppressive due to some not fully understood mechanisms. Although human body secret a lot of IgA antibodies onto the mucosal surfaces, their protective power is questionable. Some people are born with genetic defects that make them unable to produce IgA, but it only modestly increases their susceptibility to certain infections. Our respiratory tract also has a low population of memory cells. Tissue memory cells are an important first line defense against reinfections but their existence is only transient inside the lungs possibly due to the hostile environment
. There are other possible explanations proposed in the paper. Taken together, herd immunity and eradication may not be a suitable strategy when dealing with influenza, coronavirus or similar viruses.
There are good news and bad news. The bad news is that no matter how effective the vaccine is, once the virus becomes widespread, elimination is an unattainable goal and coexistence is inevitable no matter how hard we try. The good news is that even though vaccination can’t mount a durable, sterilizing immunity against these viruses, it still does an excellent job at containing the virus to the upper respiratory tract (which does not include lungs and bronchi). As a result, even if the vaccine is breached, we are most likely to experience runny nose and sore throat for a few days instead of a bad pneumonia, encephalitis, or myocarditis, etc. So a more practical strategy is slowly lifting the protective measures (masks, social distancing, etc.) after widespread vaccination and carefully monitor the viral evolution for a while until it becomes another member of minor cold virus.