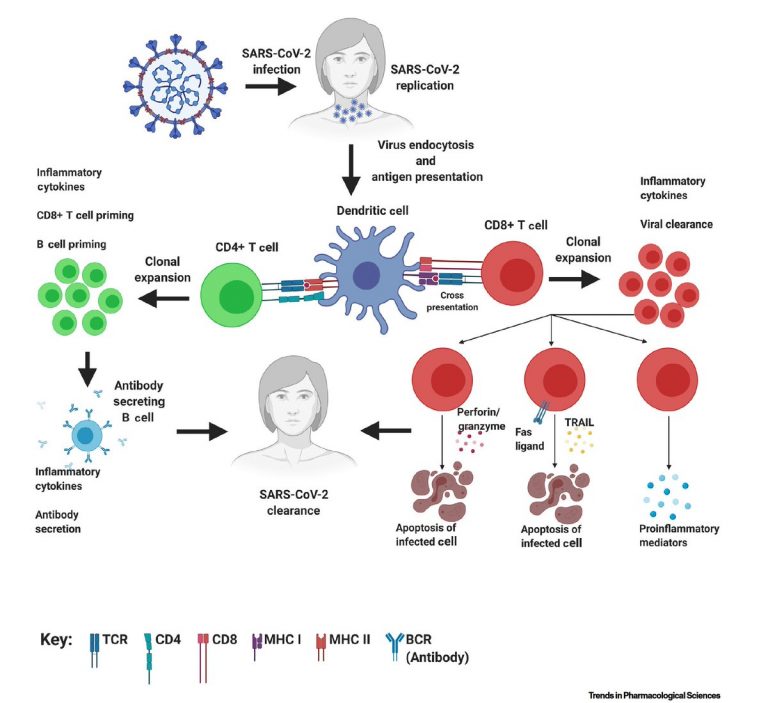
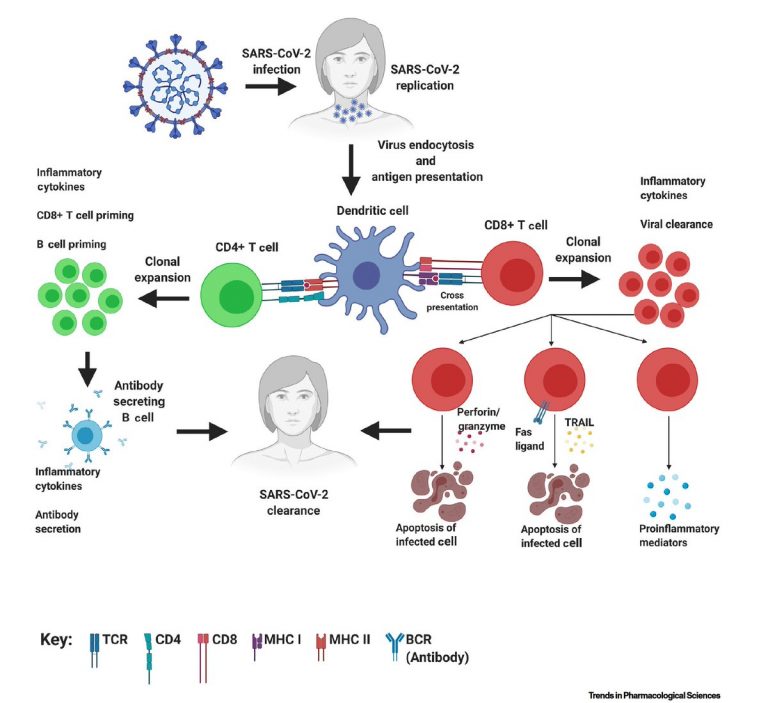
So what do we know about immunity? Basically it is provided by both T-cells and Antibodies combined.
It revolves around the T helper cells (CD4) and their ability to recognise viruses, some recognise viruses in general some corona viruses and some virus specific T cells recognise a particular virus. (VST). These are used in specific antiviral therapies.
The T helper cells trigger antibodies but also fire up the (CD8) cytotoxic cells which kill off the virus. Once the CD8 cells are circulating they differ from the amtibodies in that they are not used up after destroying the virus and move on to the next one.
There have been a few articles commenting on disappearing antibodies this is explained rather well in this article. and covers the observation that antibody presence is typically 6%. (As observed in Sweden).
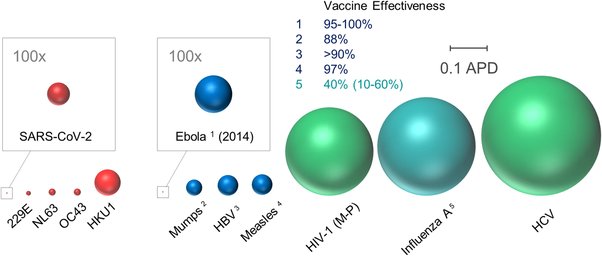
This is further complicated by the fact that even vaccines when they are developed, fully trialled and manufactured have varying ‘life spans’, Some vaccinations last for life some, like Flu vaccines may only last for a few months.
There are two things that came from background reading on this subject.
1) There area is poorly understood a present.
2) That our resistance to the virus is based on an constantly changing ‘blood soup’ of antibodies, T- cells, (many types), and blood proteins, iterferons, interleukins and other signalling proteins.
T-cell are fewer in number but don’t get used up, they repeat their function. T-cells identify the virus then trigger antibody production. Specific T-cells identify infected cells (T helper CD4) and destroy them (T killer CD8) . The number of T cells is significant Approximately 4 x 10 to the power 11 T cells circulate in the adult human body (Jenkins et al., 2009), each with multiple T cell receptors (TCR) (Varma, 2008) on its surface.
B cells and antibodies are there in large numbers, B cell can create antibodies at a rate of 2000 per second considering you can have around 10 billion B cells that’s pretty ginormous numbers but they are one hit wonders that smother the virus in the blood before they get to the cell so you need large numbers of them.
When it comes to fighting the virus this is where numbers matter:
1) If viral load is small the T-cell might destroy infected cell before the antibodies need to get going.
2) If viral load is medium then T-cells can’t cope on their own, so they trigger the antibody production. Once the infection is gone the helper cells CD4 turn off, antibodies shut down, if you didn’t test for them you might have missed them because they don’t last vey long.
3) If viral load is high the immune system goes crazy you get antibodies by the million T-cell production is high including the T-cells called CD8, cytokine killers are rampant so much so that you get a cytokine storm that damages the body, (typically lungs)
The triggers that turn all this on and off are blood proteins like Interferon and Interleukin several type s of both. Not everyone has a full quota of these so testing for them and adding and subtracting becomes the treatment.
In my troops analogy, T-helpers are the scouts, T-killers are the commandos and the antibodies are the regular the army. (There are even T gamma delta cells that destroy like crazy, the SAS of immunology).
The virus is a fast multiplier so exploits the delay in T-cell and antibody production which is as you say 2 weeks late.
Following up on this and adding a genetic rider it seems that researchers have found that there is a gene, TLR7 that is present in the X chromosome. If it is defective then the production of interferon is affected and those with the defective gene get a severe form of Covid-19.
Interferon is one of the blood proteins that turns the immune system on and off.
In males we have X and Y chromosomes, females have two X chromosomes so have a backup if one gene is defective. May be a partial explanation for why males are more affected that females by the disease.
One thing that has confused me has been how do T-cells recognise the coronavirus when its a new virus and it hasn’t seen it before? The answer is that it doesn’t need to recognise it. The reason being that the virus is already inside the cell doing its utmost to make more coronaviruses. All the T-cell needs to have previous knowledge of is how other coronaviruses behave.
How do T cells find the virus if it is inside the cell?
Here is how they do it. Once the virus has attached itself by hooking onto the ACE2 receptor on the surface of the cell it starts using its RNA to make more of itself. The ACE2 is a protein on the surface of the cell but there is a lot of activity on that cell surface with proteins moving in and out of the cell.
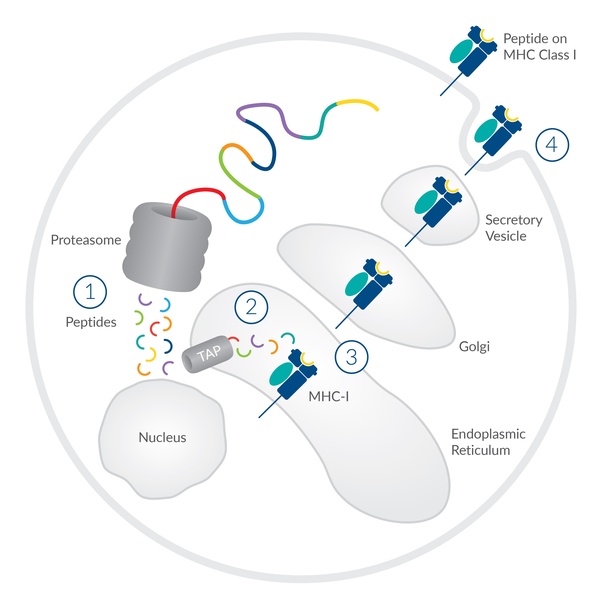
The virus makes more of itself by assembling new coronavirus by chopping up bits of protein and ordering these bits into new virus. Those chopped up bits will have a ‘signature’ by that I mean they will be different from the normal process of the cell. They are removed from the cell by a protein called MHC where they leave the cell these peptides attached to the MHC are investigated by the T cells which then suspect the cell has been hijacked and subsequently destroy it.
So the T cells unlike antibodies don’t need the full shape of the virus sipke to know what to attach to but simply know what peptide get thrown away when making a member of the coronavirus family. Pretty clever really.